Are you going through “The Change?” Hot flushes, new weight in new places, mood swings and more… It's a lot to take in. One big difference you may be experiencing is a sensitive or overactive bladder. Urinary incontinence can be an issue for menopausal women, but the good news is you don’t have to suffer in silence and there’s lots of help available.
If you’re going through the perimenopause or menopause and you’ve started to have difficulty with bladder control, you’re bound to feel concerned. After all, urinary incontinence can be embarrassing and interfere with work, your social life and your sexual relationship. Unless you find the right incontinence products and solutions for you.
Never Lose Hope!
However, it’s important to understand that urinary incontinence isn’t something you ‘just have to put up with’. As Dr Sarah Jarvis says “Menopause used to be the start of an inevitable decline into old age – but no more!” Urinary incontinence can be cured, treated or at least better managed. What you don’t want to do is ignore the problem, as it rarely goes away on its own and may even get worse over time.
Instead, educate yourself about why you may be experiencing bladder leaks and how they are connected to your menopause symptoms. Here are the symptoms, some reasons why they occur, and what you can do about bladder leaks.
Types of Menopausal Incontinence
Bladder leaks during the menopause are typically symptomatic of one of two different types of incontinence: stress incontinence or urge incontinence.
Stress incontinence is the result of a weakened pelvic floor, the system of muscles, ligaments, and tissue that support your bladder and uterus. Once weakened, pressure – or stress – put on the pelvic floor by everyday activities like laughing, sneezing, coughing, or exercising leads to a little bladder leak. As women, we may go through lots of experiences during life that can weaken our pelvic floor, such as pregnancy, childbirth, hormonal changes, or gaining weight.
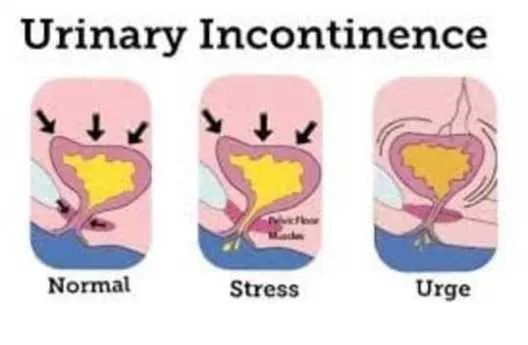
Urge incontinence is a result of declining oestrogen levels, muscle or nerve damage in the bladder tissue caused by past pelvic surgery, such as a C-section, or a neurological disease, such as multiple sclerosis or Parkinson’s. As a result, the bladder muscles involuntarily spasm, creating frequent intense and sudden urges to urinate that send you running to the toilet. You may or may not make it to the toilet on time.
Symptoms of Menopausal Incontinence
Are you experiencing these common signs of a menopausal sensitive bladder?
-
Leaking urine when you cough, sneeze or exercise
-
Leaking urine on the way to the toilet
-
Waking up more than twice a night to urinate
-
Frequent urinary tract infections
If you’ve started noticing any of these signs, it would be a good idea to make an appointment for a chat with your GP.
Common Causes of a Menopausal Sensitive Bladder
Here are some of the reasons why you may be experiencing urinary incontinence during menopause.
-
Weak pelvic floor muscles. During menopause, your pelvic floor muscles tend to weaken naturally. Weaker muscles can mean less bladder control and more frequent urination in women.
-
Prolapse. A prolapse is a sagging down of organs against the pelvic floor. Some women who have prolapse describe a feeling of a lump in the vagina where an organ is sagging down. That organ may be the uterus, bladder or bowel. Prolapse strains your pelvic floor.
-
Less bladder elasticity. The base of your bladder can lose elasticity and have trouble stretching to accommodate your urine as it fills. As a result, your bladder is irritated as it fills, causing an “overactive bladder” sensation that makes you feel like you have to go more frequently.
-
Oestrogen depletion. With the onset of menopause, oestrogen is no longer produced by your body. When this happens, your body is more susceptible to incontinence because there isn’t enough oestrogen to help keep the tissues around your bladder strong and working well.
-
Weight gain. Many women tend to gain weight during menopause. Since your pelvic floor muscles support much of your body weight, any excess weight further strains these muscles, so they cannot support your bladder as they should.
Managing Your Urinary Incontinence
The first thing you should do if you’re having any problems is book a chat with your GP who’ll be able to offer lots of help and advice.
A great first step is strengthening your pelvic floor muscles with pelvic muscle contraction exercises. Strengthening your pelvic floor will help you increase control over little bladder leaks. Kegel or pelvic floor exercises can be a huge help and can be done pretty much anytime and anywhere.
Try your best to stay around your normal healthy weight. Excess pounds put pressure on your pelvic floor and can cause your bladder to leak when you laugh, sneeze or cough.
Be sure to stay hydrated. Not only will this help guard against urinary tract infections, but it will keep your urine from becoming too concentrated and acidic.
Other urinary incontinence remedies to try include adopting a bladder-friendly diet by avoiding foods like caffeine, alcohol, chocolate, citrus fruit, and carbonated drinks as they make your urine more acidic, which can further aggravate an already sensitive bladder. You may also want to create a ‘go’ schedule. Visiting the toilet on a fixed schedule can bring some predictability as well as ease your urinary urgency. Start by going to the toilet every two hours, whether or not you feel the urge to go, and adapt from there.
Will trying these management methods work? That depends on the cause of your incontinence. That’s why it’s so important to start talking to your doctor early. He or she can help with diagnosis and additional treatment options if you need them. For example, you can also ask your doctor about bladder training or surgeries to treat prolapse and other underlying conditions that contribute to your overactive bladder.
To feel confident and fresh even as bladder leaks happen, try Always Discreet incontinence liners, Always Discreet incontinence pads, and Always Discreet underwear. They offer amazing move–all–you–want sensitive bladder protection. The liners and pads have a thin and flexible design for light to moderate protection and our feminine, discreet urinary incontinence underwear has double LeakGuards™ to help stop leaks where they happen most – at the legs. For bad leaks at night, try the underwear –which is so much better than having to use a bed pad!
Whatever course you take, remember one thing: many women face bladder control issues at this stage in life. But with sensitive or overactive bladder and some poise, you don’t have to let it get in the way of life, love and a great time!
*If you are going through menopause or experiencing bladder leaks, always make sure to consult your doctor or a health specialist for these medical conditions.
*Always Discreet products are not products to help with menopause, but medical devices for bladder leaks, which may be a symptom experienced by some women during menopause.